While it is the surgeon’s task to make medical decisions and perform surgeries, it is the responsibility of assistants and technicians to make sure their surgeon has appropriately maintained instruments, devices, and supplies to perform the surgery. This article will identify the common instruments (Table 1, page 18) and in-office procedures used in glaucoma practices, as well as safe disinfection practices and proper processing procedures.
| INSTRUMENT | WHAT IT DOES |
|---|---|
| Caliper (Castroviejo or Braunstein are common models) | Measures distances |
| Cannula | Carries fluid, such as balanced salt solution or viscoelastic |
| Forceps with teeth | Grasps tissue with a fine tip |
| Forceps without teeth | Grasps tissue with a smooth-edged tip to avoid puncture |
| Foreign body/corneal spud | Removes superficial corneal foreign bodies and applies posterior pressure for a paracentesis |
| Needle holder | Holds suture needle firmly in position while applying sutures; locking or non-locking, depends on surgeon’s preference |
| Speculum | Keeps eyelids open and eyelashes out of the operating field |
| Tying forceps | Grasps and maneuvers suture material |
| Vannas scissors*Mostly used in the OR though some offices use them for in-office postoperative procedures | Cuts, via small slender blades, curved or straight depending on surgeon’s preference, one sharp and one blunt blade |
| Westcott scissors | Cuts, via curved, medium blades with blunt tips |
| Note: This list is not all-inclusive as every physician practices differently and has different facilities available to perform procedures. | |
Six common in-office procedures used in a glaucoma practice
Laser procedures. Laser procedures to treat glaucoma in the practice include laser peripheral iridotomy (LPI), selective laser trabeculoplasty (SLT) and laser suture lysis (LSL). These procedures are designed to make a small burn or opening in the eye tissue to allow for better drainage of fluid. The most commonly used lenses in these procedures are the Abraham iridectomy for LPI, Latina for SLT, and Blumenthal for LSL.
 In-office bleb revision or “needling.” During a trabeculectomy, a channel with a trap door on the sclera is formed, allowing aqueous to drain out of the anterior chamber into a pocket of fluid called a “bleb.” Scarring of the trap door and bleb (bleb failure) can prevent aqueous from draining out of the eye, increasing eye pressure.
In-office bleb revision or “needling.” During a trabeculectomy, a channel with a trap door on the sclera is formed, allowing aqueous to drain out of the anterior chamber into a pocket of fluid called a “bleb.” Scarring of the trap door and bleb (bleb failure) can prevent aqueous from draining out of the eye, increasing eye pressure.
The bleb needling procedure cuts the scar tissue and frees the trap door and bleb, re-establishing aqueous flow into the bleb and decreasing intraocular pressure (IOP). Needling is often accompanied by an injection of an antifibrotic agent, such as 5-fluoracil or mitomycin-C. Each surgeon uses different instruments for their version of this procedure but scissors, a needle holder, a speculum, and forceps are commonly used.
 Anterior chamber paracentesis (ACP). ACP provides a controlled drainage of the aqueous humor from the anterior chamber by using a needle or a paracentesis incision. This can be done by using a slit lamp under topical anesthesia and aseptic conditions. ACP is repeatable and has the advantage of rapid IOP reduction.1 ACP is commonly used to quickly reduce IOP post-cataract or glaucoma surgery, to take samples of aqueous for pathology investigation in cases of infection or suspicion of malignancy, and to temporarily reduce pressure from moderate to severe hyphemia prior to surgery in the OR. While some surgeons prefer to use a needle to aspirate aqueous, others may prefer a cannula. A speculum is commonly used.
Anterior chamber paracentesis (ACP). ACP provides a controlled drainage of the aqueous humor from the anterior chamber by using a needle or a paracentesis incision. This can be done by using a slit lamp under topical anesthesia and aseptic conditions. ACP is repeatable and has the advantage of rapid IOP reduction.1 ACP is commonly used to quickly reduce IOP post-cataract or glaucoma surgery, to take samples of aqueous for pathology investigation in cases of infection or suspicion of malignancy, and to temporarily reduce pressure from moderate to severe hyphemia prior to surgery in the OR. While some surgeons prefer to use a needle to aspirate aqueous, others may prefer a cannula. A speculum is commonly used.
 Sub-Tenon’s injections. A steroid injection is used to decrease inflammation, swelling, or leaky blood vessels inside the eye. The injection is between the sclera and Tenon’s capsule. This capsule is a sheet of connective tissue between the globe and the orbit that provides a smooth socket allowing free movement of the globe. This pathway permits a prolonged contact time of the drug with the sclera. The medication acts to decrease inflammation and leakage from blood vessels from a variety of causes, thereby offering the opportunity for improvement in vision. A speculum and injection supplies are needed.
Sub-Tenon’s injections. A steroid injection is used to decrease inflammation, swelling, or leaky blood vessels inside the eye. The injection is between the sclera and Tenon’s capsule. This capsule is a sheet of connective tissue between the globe and the orbit that provides a smooth socket allowing free movement of the globe. This pathway permits a prolonged contact time of the drug with the sclera. The medication acts to decrease inflammation and leakage from blood vessels from a variety of causes, thereby offering the opportunity for improvement in vision. A speculum and injection supplies are needed.
 Suture placement. Wound leak sutures (cornea) and bleb needling sutures (conjunctiva) are the most common. A needle holder, suture, a fluorescein strip and Weck-Cel are needed. Most surgeons prefer to place sutures in a procedure room with the patient lying down, while some surgeons prefer to do this at the slit lamp.
Suture placement. Wound leak sutures (cornea) and bleb needling sutures (conjunctiva) are the most common. A needle holder, suture, a fluorescein strip and Weck-Cel are needed. Most surgeons prefer to place sutures in a procedure room with the patient lying down, while some surgeons prefer to do this at the slit lamp.
 Suture removals. Removing a suture from the cornea, conjunctiva, or an occluding suture from a Baerveldt tube (ripcord maneuver). Some surgeons prefer a simple disposable blade and a pair of Jewelers forceps, while others may request a pair of Vannas scissors or a suture needle locked into a needle holder to cut the suture. Each surgeon has her own preference.
Suture removals. Removing a suture from the cornea, conjunctiva, or an occluding suture from a Baerveldt tube (ripcord maneuver). Some surgeons prefer a simple disposable blade and a pair of Jewelers forceps, while others may request a pair of Vannas scissors or a suture needle locked into a needle holder to cut the suture. Each surgeon has her own preference.
Examples of glaucoma instruments



Courtesy of Bausch+Lomb

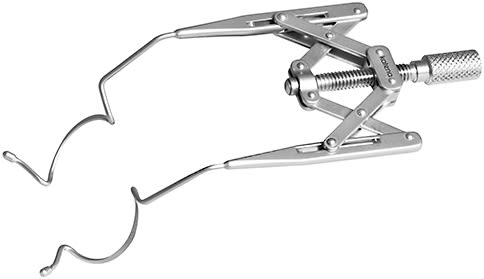

Courtesy of Katena
Safe disinfection practices
The American Academy of Ophthalmology has reported that transmission of infectious agents could occur from failure to adequately disinfect ophthalmology devices.2 Infectious agents that could be transmitted include, but are not limited to, pseudomonas aeruginosa, acanthamoeba, methicillin-resistant staphylococcus aureus, or MRSA, and fungi.
If not disinfected or sterilized correctly, instruments could be the cause of endophthalmitis or toxic anterior segment syndrome (TASS), an acute, noninfectious inflammation of the anterior segment of the eye. Various contaminants, usually from surgical equipment or supplies, have been implicated as causes of TASS.3
At a minimum, use high-level disinfection for any items, such as laser lenses, that touch mucous membranes, such as the eye. Items that come into contact or enter sterile tissues, such as instruments used for surgical procedures or that touch an ulcerated cornea, must be sterilized.4
Offices can use the following safety actions to protect patients from the risk of infection associated with tonometers, laser lenses, and other ophthalmology devices:
- Make policies and procedures readily available in writing to all staff responsible for disinfecting items.
- Update policies annually or as new chemicals and instruments are introduced to the practice.
- Review cleaning and disinfection instructions for use of eye instruments to ensure they are being reprocessed appropriately.
- Ensure disinfectants listed as compatible, other than bleach, are FDA-approved high-level disinfectants. Manufacturers often list products as compatible that may be used for pre-cleaning. Some of these products may be commonly available surface disinfectants but are not effective as high-level disinfectants.
- Keep and follow manufacturer instructions for use for both the devices used for ophthalmology examinations and procedures, as well as cleaning and disinfection products. This includes lenses used for laser procedures and for tonometer tips.
- Ask an individual who has knowledge about different types of disinfectants to review the product label and instructions for use. If instructions are unclear, technical services for the manufacturer of the item and any products used in conjunction with reprocessing should be contacted.5
Proper processing procedures
- Wear appropriate personal protective equipment when processing instruments.
- Follow the manufacturer’s recommendations for sterilization, such as steam, ethylene oxide, or immediate-use steam sterilization.
- Allow adequate time for processing instruments according to the manufacturer’s instructions; otherwise, cleaning and sterilization will be ineffective.
- Identify a designated cleaning area and equipment specific to the cleaning of ophthalmic surgical instruments.
- Pre-clean instruments immediately following use.
- Use only those cleaning agents the manufacturer recommends.
- Per the American Society of Cataract and Refractive Surgery TASS Task Force, a non-enzymatic cleaner is recommended for disinfection of all ophthalmic instruments, because previous studies have shown that enzymatic residues on intraocular instruments are a leading cause of TASS.5
- Pay particular attention to the specified concentration and pH of the cleaning agent, as well as the recommended water quality.
- Perform final rinsing of the instrument with sterile, distilled, or deionized water, unless otherwise specified by the manufacturer.
- Properly maintain cleaning and sterilization equipment.
- For any instrument that could potentially pierce through a standard autoclave pouch, place a tip protector over the whole blade or jaws of the instrument.
- Do not pack multiple instruments together in pouches. Places where metal touches other metal will not be sterilized.
- Never stack instruments — store upright and in chronological order of sterilization.
- Reprocess any instrument that has not been used in the last 6 months.
- Keep a log of which instruments are processed each day.
Not just in the surgeons’ hands
The difference between success and failure of surgery for open-angle glaucoma is of the greatest magnitude. When the ideal surgical results are achieved, the patient may have lifelong clear media, good visual acuity, and complete control of the glaucomatous process without visual field loss. If an unfavorable course ensues, the patient may lose the best opportunity for a good result, for the prospect of success will never be as good again with later operations
These seemingly simple steps can help keep your patients safe from serious infections and catastrophic postoperative complications. OP
References
- Benefits of anterior chamber paracentesis in the management of glaucomatous emergencies 2014 – M Cioboata, A Anghelie, C Chiotan, R Liora, R Serban, and C Cornăcel https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391354/ Accessed 3/1/2020
- Failure to High Level Disinfect Ophthalmology Devices Leading to Transmission of Infectious Agents May 2019 - Sylvia Garcia-Houchins, MSN, RN, CIC, director, Infection Prevention and Control https://www.jointcommission.org/resources/news-and-multimedia/blogs/on-infection-prevention-control/2019/05/failure-to-high-level-disinfect-ophthalmology-devices-leading-to-transmission-of-infectious-agents/ Accessed 3/1/2020
- Toxic anterior segment syndrome (TASS) after Cataract surgery 2006 - Mamalis N, Edelhauser HF, Dawson DG, Chew J, LeBoyer RM, Werner L. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5625a2.htm Accessed 3/1/2020
- ASCRS, AAO, and OOSS release joint recommendations on the use of enzyme detergents to clean intraocular surgical instruments January 2016 - Liz Hillman EyeWorld Staff Writer https://www.eyeworld.org/article-ascrs--aao--and-ooss-release-joint--recommendations-on-the-use-of-enzyme--detergents-to-clean-intraocular Accessed 3/1/2020
- Guidelines for the Cleaning and Sterilization of Intraocular Surgical Instruments 2018 - ASCRS, OOSS, AAO Hoskins Center for Quality Eye Care https://www.aao.org/clinical-statement/guidelines-cleaning-sterilization-intraocular Accessed 3/1/2020









