6th Annual Reader Survey

Numbers don’t lie. Sometimes, however, they don’t tell the whole story. That’s certainly the case with this year’s Ophthalmic Professional Reader Survey.
The survey collected reader responses for more than a month spanning March and April. Of course, as the numbers for COVID-19 grew during this time, the world took a dramatic turn. On March 18, the American Academy of Ophthalmology responded to the pandemic with the recommendation that all ophthalmologists “immediately cease providing any treatment other than urgent or emergent care.” Responding to the pandemic, the re-opened practice of today is not the practice of March, and time will tell which data from the survey will hold true in our new reality.
To paint a full picture of the profession, OP reached out to a representative mix of ophthalmic and allied health professionals to see where their businesses — both large and small — stand as of mid-June.
Here is a look at some of the early 2020 survey statistics and how they compare to the new reality, as described by six ophthalmic professionals. They are:
- Barbara Cardelli, administrator at Advanced Surgical and Medical Eyecare, a single ophthalmologist practice at The Villages, a retirement community of 50,000 residents in central Florida
- Carol Olvera, COT, and Michelle Wagner, OSC, clinical managers at Colorado Retina with five Denver metro locations and one satellite office
- Lynn Girdlestone, COA, OSA, OSC, a training consultant and certified ophthalmic assistant at The Everett Clinic in Northwest Washington State with a main hub for ophthalmology and four satellites for optometry
- Zora Harrison, COE, chief operating officer at Ocala Eye, with six locations in the Ocala, FL, area
- Savory Turman, COMT, OCS, clinical director at Eye Center of Northern Colorado in Fort Collins, CO, with six clinical sites and two surgical facilities.
Practice status
Most of the ophthalmic professionals interviewed report their practices reopened in May, after providing very limited services during the quarantine. Several also report that a number of visits were done remotely through telehealth.
“We did telehealth,” says Ms. Cardelli. “Though staff was furloughed, our doctor and one technician ‘Zoomed’ with patients,” referring to the web-based video conferencing tool Zoom.
Ocala Eye was open for emergencies and for patients who needed emergent care. Specifically, Ms. Harrison, reports: “We also introduced telemedicine and drive-up IOP testing at all of our locations.”
Some practices remained open only at certain locations. Ms. Olvera says all but one of Colorado Retina’s offices “stayed open for emergency and urgent treatment only. We’re gradually reopening, but patients can still schedule telemedicine video conferencing appointments.”

SURVEY METHODOLOGY
The Ophthalmic Professional Reader Survey was conducted online beginning on March 13. Emails invited subscribers to participate. Readers also were prompted to take the survey via links on OP’s website and social media. OP received 344 total responses. Of those, 95 respondents were disqualified, as they did not indicate they maintain a full-time allied health position in an ophthalmology practice. The survey closed on April 12. Respondents were entered in a drawing for one of five $100 American Express gift cards, won by Shone Boyer, Lynn Haven, FL; Myra Cherchio, Palm Harbor, FL; Stacey Lewis, Pensacola, FL; Sue Lundgren, Salisbury, NC; and Kyle Plouhar, Fruitport, MI. All individual responses are confidential.
Eye Center of Northern Colorado was closed from mid-March until early May, except “for urgent and emergent cases in two of our six clinical sites and our two surgical facilities,” says Ms. Turman.
Ms. Girdlestone reports: “We shut down all of our optometry offices and funneled all triage situations to one MD with three technicians each day in the office.”
The Everett Clinic reopened May 5 at half capacity “to accommodate social distancing,” says Ms. Girdlestone. “As the weeks go by, we will slowly ramp back up.”
Reopening isn’t easy, however. As Ms. Cardelli explains, “Our first full week was in late May, and we’re trying to adjust as we go along. We were in the office two weeks prior to get everything ready.”
Commitment to the profession
As practices reopen, they are also bringing back employees in various capacities. In doing so, they are recalling a workforce that is committed to both the profession and the practice. Whereas the typical American professional has been with his or her employer for 4.2 years, according to the Bureau of Labor Statistics, only 3.51% of respondents to this survey have been with their current employer for less than six years. More than 35% have been in an ophthalmic-related position for more than 30 years (See Figure 1).
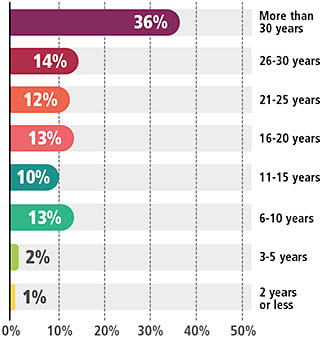
Among the six ophthalmic professionals interviewed here, Ms. Cardelli has worked in ophthalmology for 41 years; all of the professionals interviewed here have been with their current employer for at least five years.
This year’s survey pointed to a slight increase in new professionals to the category, but it is too early to tell the degree to which those hiring and longevity trends change in this evolving environment.
As Ocala Eye’s Ms. Harrison puts it: “Staffing is a challenge in general. Throw in a global pandemic, and now you have a perfect storm.”
Approaches to staffing
Those interviewed stress that allied health professionals are essential to surviving this storm. For example, Everett Eye’s four locations boast 29 technicians plus eight opticians. Among Colorado Retina’s 200 employees, clinic managers Ms. Olvera and Ms. Wagner work with 65 staff members.
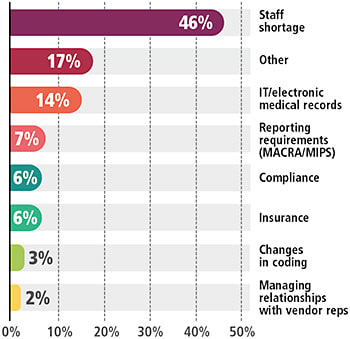
Though 46% of respondents to the OP survey reported staff shortage has increased their workload, the pandemic has closed most doors to hiring right now (See Figure 2).
“Because of the safety precautions,” explains Ms. Cardelli, “we are seeing [fewer] patients at Advanced Surgical and Medical Eyecare. As a result, we reduced our medical department by one employee.”
“While we were closed,” adds Ms. Girdlestone, “those not physically in clinic were paid to stay home and be on-call. Eventually, our leadership team established ways for us to work from home on rescheduling patients for our providers and checking on patients who needed it.”
While some practices kept staff on hand, some did not. “Our practice,” explains Ms. Harrison, “chose to keep all of our staff fully employed during this time. We allowed staff to work from home and rotated our allied health professionals to serve in clinics when needed. All staff received full hours despite the reduced workload. Staff worked very hard to share the workload and ensure all patients were properly cared for.”
For some, funding, such as that offered by the Small Business Administration, was a help.
“Our staffing needs dropped dramatically,” explains Ms. Turman. “We were able to provide a couple of additional PTO weeks for our team. We then did a furlough so staff could maintain health insurance and were able to bring team members back with the SBA loan.”
For other operations, it was time to tackle the never-ending to-do list.
“We went down from having 11 doctors in the offices every day to having just four, one at each location,” explains Ms. Olvera of Colorado Retina. “We were severely overstaffed for what our clinical needs were, but we were able to use the time well. We did a lot of remote training. Our doctors who weren’t working volunteered their time to do follow-up training for staff.”
Ms. Wagner says the practice even found new needs for which sidelined employees could fill. “We were able to utilize some employees in what we call the greeter position, located outside to take temperatures and ask pertinent medical questions to make sure patients should be coming into the practice at that time.”
At Ocala Eye, Ms. Harrison says they were able to adjust job descriptions of some employees to fit new needs of the practice.
“We quickly converted our practice ... implementing mobile check-in services as well as virtual prescreening work-ups to reduce the amount of time the patient was in our office. In terms of staffing needs, this requires more employees and longer hours.”
New expectations?
How is the pandemic impacting hiring and training to meet changing staffing needs?
“As a large employer,” says Ms. Harrison, “it is important to our owners to keep staff employed. We do not have plans to adjust our staffing other than do more cross training of positions.”
Training and/or retraining are key for several of the ophthalmic professionals we interviewed.
“Our needs have not really changed,” explains Ms. Girdlestone. “We are fully staffed for each provider and have floats available if someone calls out.”
At Colorado Retina, Ms. Olvera thinks the patient greeter position will become permanent, at least for the foreseeable future.
42% of respondents indicate their bonus was determined by individual performance. “How was your bonus determined?” was a new question this year.
“We need one person in that position in each of our offices.”
As for technicians, she adds, “I don’t see our needs changing much. However, we may need to hire scribes, for example, because our doctors don’t want them working for multiple physicians because they work so closely together.”
Evaluating the job market
With some positions changing in many offices, do practices expect a shortage of allied health professionals moving forward?
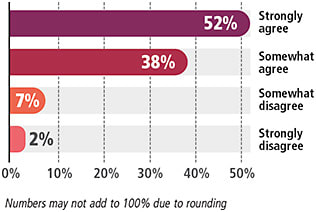
In the annual survey, 52% of respondents reported they strongly agree that their workload has increased in the last year (See Figure 3). Nearly half (46%) said a shortage in staff was the major contributing factor (See Figure 2).
However, none of the ophthalmic professionals interviewed see increases in hiring, except to replace vacant staff positions.
“Everybody is doing what we are,” explains Ms. Cardelli. “That is, looking to see where you can do with one less employee here or there. In our area, we see scribes and technicians bouncing around a lot.”
“I think what really is going to suffer, as it does in any downturn, is middle management,” adds Ms. Cardelli.
In larger practices, middle techs, or those who spend less time, if any, seeing patients and instead perform tasks like scheduling, paperwork, and training, will be the first to go, she elaborates. Ms. Cardelli advises that the best way to insure against this is to stand out and be the best through tasks furthering your education, brushing up on your technician or customer service skills, reducing workup time to be within benchmark, etc. “Plus, I think a lot of practices will be afraid to expand or even go back to the way they operated before this,” she adds.
“The needs of my clinic will likely not change,” adds Ms. Girdlestone. “In the eyecare industry as a whole, however, there is a shortage of allied ophthalmic professionals. Experienced technicians are becoming scarce in our region, and I anticipate that will get worse as our generation will see high demand for nurses, doctors, and other essential positions in the coming years.”
Ms. Turman agrees. “We were hiring prior to COVID-19 due to anticipated staffing needs and are now as well. There is definitively a shortage of trained staff, and there has been for years. We now envision difficulty finding medical personnel since hospitals and general practice settings are facing staffing issues as well, and they often offer higher salaries.”
A snapshot of compensation
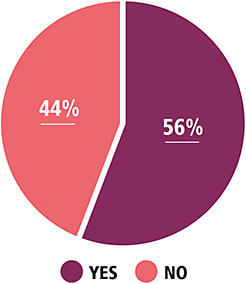
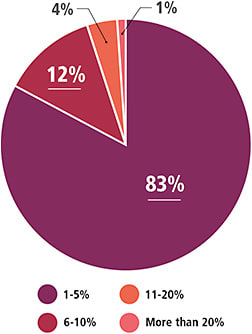
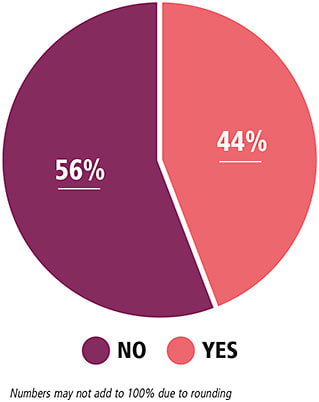
What about salaries? Before the pandemic, 56% of allied health professionals reported an increase in salary. Of those respondents, 83% reported an increase in the range of 1-5% (See Figure 4 and Figure 5).
So, what measures will practices be taking going forward?
The annual survey found that 44% of respondents were being compensated with bonuses. That represents an increase from 2018, but a slight decrease from 2019, when 46% of respondents reported receiving bonuses (See Figure 6).
Today, just a few week later, bonuses are on hold for the foreseeable future, report those interviewed.
“At this point, we have frozen them,” says Ms. Wagner.
Regarding her single-ophthalmology practice, Ms. Cardelli points out that, “We did a COVID bonus with our PPP money, but any other changes will depend on where we are and what it looks like after we all get through this. We’ll have to see if we’re making enough revenue to keep afloat the same way we are operating now. Who knows where we’ll be in six months?”

SUPPORT STAFF
It’s never been more important to show support for staff, says Colorado Retina’s Michelle Wagner. “Check in with your technicians individually ... about their mental health, their families, and if there’s anything we can do to provide extra support during this period. They really seem to appreciate one-on-ones and talking to us more deeply, whether it’s home- or work-related.”
“That’s something we routinely do at least one a month,” adds co-clinical manager Carol Olvera. “We have 65 staff members reporting to us, so keeping up with that has been really important, even if it was done virtually during this period.”
Put another way: “We have been forced out of our comfort zone, and I believe we are better for it,” says Ocala Eye’s Zora Harrison.
“I do not see an increase in compensation any time soon,” adds Ms. Girdlestone of The Everett Clinic.
However a practice handles it, recovery requires creativity, says Ms. Turman. “We have been seeking ways to meet our patient demands while balancing staffing limitations through creative scheduling, extended hours, and cross-training team members in administrative tasks. We will be limited on increasing salaries, etc. until we are able to recover more financially.”
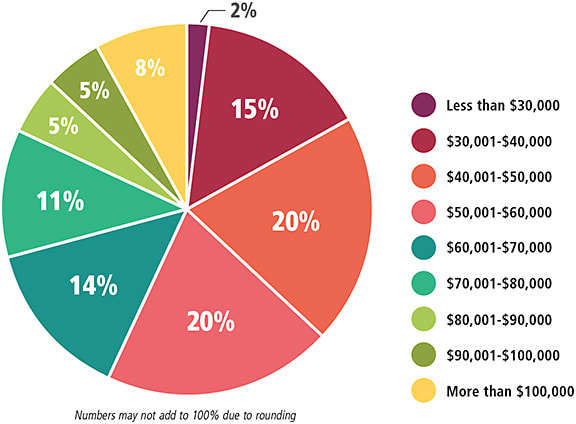
Speaking of salary, the data collected for the 2020 survey are relatively similar to data from previous years, with both $40,001-$50,000 and $50,001-$60,000 salary ranges represented by about 20% of respondents (See Figure 7).
Value of certification
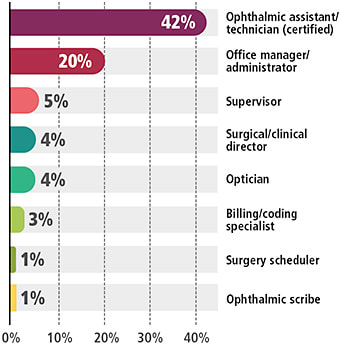
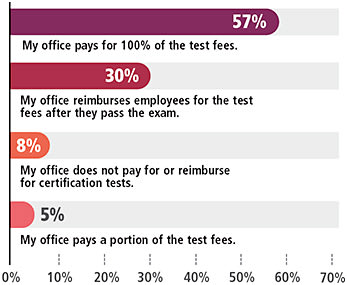
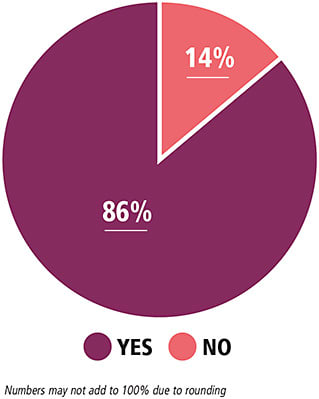
Among survey participants, 42% say they are certified assistants/technicians. Nearly nine out of 10 respondents (86%) report their offices pay for recertification, with 57% covering all test fees (See Figures 8-10).
88% say their office pays for continuing education.
No one interviewed for this article sees the importance of certification decreasing. Ms. Cardelli echoes these sentiments: “Certified staff is definitely more valuable.”
Ms. Harrison agrees, adding: “Once we find the right talent, we invest in certification.”
What else makes an employee valuable to the practice? These days, flexibility is key, too. “Especially during these times, the thing that really makes an employee valuable is being adaptable,” Ms. Wagner says.
Conclusion
So, is any silver lining to all of this?
“If this pandemic has taught me anything, it’s that in-person eye care isn’t going anywhere any time soon,” Ms. Girdlestone says. “While we may be able to high-level triage with video visits, it’s not the same as sitting someone down at a slit lamp. And, someone’s unexpected visual field cut cannot be truly measured without a visual field machine.”
The bottom line: “Eye doctors will always be needed, and so will their technicians, opticians, and office staff,” Ms. Girdlestone says. OP









