Cornea
Dry eye and MGD 101
Part five of a seven-part corneal/anterior segment survival guide.
BY KENDRA DAVIS, COA
The Report of the International Dry Eye Workshop (DEWS), published in 2007, defines dry eye as a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface.1 It is accompanied by increased tear osmolarity and inflammation of the ocular surface. A smooth corneal surface is necessary to maintain clarity in vision, so dry eye may result in blurry vision.
Cornea and tear film
The average adult cornea measures about 1/2 mm thick (540 microns).2 The cornea provides a major part of the refractive power in the eye and is comprised of five layers:2
1. Epithelium
2. Bowman’s membrane
3. Stroma
4. Descemet’s membrane
5. Endothelium
The tear film covers and protects the cornea.2 An inadequate amount of tears or poor quality of tears can result in dry eyes.2 Additionally, the tear film is compromised due to daily exposure to environmental irritants and exacerbating behaviors such as computer usage and reading, which decrease blink rate.
A stable tear film is required to maintain a healthy ocular surface, comfort, and visual clarity. It serves to lubricate the eye, protect against infection, keep the vision clear, and wash away foreign particles. Dry eye, also known as keratoconjunctivitis sicca, is becoming a more commonly diagnosed ocular condition. The American Academy of Ophthalmology suggests that about 3 million people suffer from this condition.

Figure 1: Measuring elevations in a patient’s MMP-9 enzymes using RPS’ InflammaDry gives us an objective assessment of inflammation.COURTESY BASCOM PALMER PHOTOGRAPHY
Common ocular symptoms include:
• Scratchy eyes
• Tearing
• Blurred vision
• Light sensitivity
• Foreign body sensation
• Burning
Each component of the tear film serves a purpose. The outermost layer, the lipid layer, provides a sealant to keep the tears from evaporating.3 The middle layer, the aqueous layer, carries vitamins, minerals, and salt to the cornea.3 The innermost layer, the mucin layer, helps to nourish the corneal surface, ensuring that the tears spread evenly over the surface.3
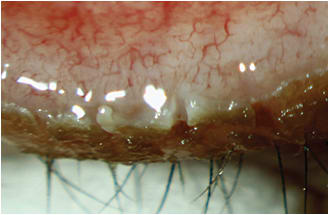
Figure 2: A patient with chronic meibomian gland dysfunction.COURTESY BASCOM PALMER PHOTOGRAPHY
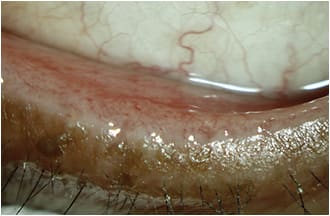
Figure 3: Post-lid debridement, manual expression and lid cleaning.
The lacrimal glands in the palpebral conjunctiva in the upper eyelid and superior conjunctival fornix produce the aqueous (middle) layer portion of the tear film. When blinking, the upper and lower lids meet, allowing the meibum to secrete from the meibomian glands posteriorly onto the ocular surface.3 An incomplete blink may result in exposure keratitis, inferiorally.
What is meibomian gland dysfunction?
Our meibomian glands sit on the posterior lash line of the upper and lower lids. The tarsus contains the meibomian glands. The upper lid contains 25-30 glands and the lower lid contains 20-25 glands. The glands are responsible for secreting lipids of the tear film onto the corneal surface. Meibomian gland dysfunction (MGD) is a condition that often goes undiagnosed. Proper diagnosis of dry eye syndrome and, more specifically, identification of MGD is essential to providing appropriate treatment. Partial blinking increases blockage of the glands, resulting in thickening of the oil layer as well as obstructing the glands, resulting in MGD.
Assessment
When patients present with ocular signs and symptoms such as burning, stinging, and sharp pains of the eye, the technician should initiate an assessment with a patient survey such as the Ocular Surface Disease Index (OSDI). Using the patient’s responses, the OSDI indicates the subjectivity of symptoms, which helps the doctor diagnose dry eye syndrome. The physician and/or physician extender must also take into consideration the patient’s age, gender, medications (systemic and ocular), medical conditions, and chronic environmental conditions or exposures, which may be work-related.
After identifying ocular surface disease, the physician’s examination begins with a complete dry eye evaluation (including assessment of meibomian gland dysfunction). External slit lamp examination of the ocular surface is pivotal before undergoing ocular surgery. Ocular surgery may alter the ocular surface, predisposing our surgical patients to post-operative dry eye complaints. The physician must decipher if the patient is experiencing aqueous deficiency, evaporative dry eye, and/or a combination of the two well-known subtypes of dry eye disease: aqueous deficient and evaporative.
Diagnosis
We use several tools to perform our dry eye assessments, including the following:
• Osmolarity Test (TearLab). Measures the solute level in the tear film.
• InflammaDry (Rapid Pathogen Screening, Inc.). Immunoassay gives us an objective assessment of inflammation by measuring elevations in matrix metallopeptidase 9 (MMP-9) enzymes.
• Lipiview II (TearScience). Measures the absolute thickness of the tear film lipid layer, provide high-quality digital imaging, and identifies partial blinking as well as archive assessment of the meibomian glands.
• Observe lid structure and manual meibography.
• Corneal fluorescein staining.
• Conjunctiva lissamine green staining.
• Evaluating the glands manually by expression of the glands.
• The Korb Meibomian Gland Evaluator (TearScience). A standardized device used to evaluate the meibomian gland function.
• LipiScan (TearScience). High-definition diagnostic imaging of the meibomian gland.
Clinical advancement
Clinical therapy options for dry eye syndrome and MGD include:
• LipiFlow (TearScience). Uses thermal pulsation, a minimally invasive technique that massages the oils from the meibomian glands.
• MiBo Thermoflo. Uses a thermoelectric heat pump to liquefy the meibum to facilitate expression of gland secretions.
• Manual expression. Warm compresses to the lids with digital massage of the glands.
In addition, patients can take advantage of many home therapy options. These options include:
• Warm compress
• Lid hygiene
• Topical antibiotics
• Oral supplements
• Blinking exercises
• Preservative-free artificial tears
• Moisture-release eyewear
• Sleep eyewear goggles and mask
Conclusion
When evaluating a patient for dry eye disease, take the time to visually examine the whole patient prior to slit lamp exam. Listen to their signs and symptoms as well as to time of onset. Each patient will present differently, therefore you will need to cater to each patient as an individual.
I recommend to patients that they take note of when they most commonly experience ocular discomfort and pain. Once patients are diligent with some form of clinical therapy in addition to home therapy, they notice improvements commonly lasting from one to three months. OP
References
1. International Dry Eye Workshop. The definition and classification of dry eye disease. Report of the International Dry Eye Workshop (DEWS) 2007:75-76.
2. Eyelid Anatomy and Function. Lin LK. May 2013. Ocular Surface Disease: Cornea, Conjunctiva and Tear Film. Elsevier:11-15.
3. Stern ME, Beuerman RW, Pflugfelder SC. The normal tear film and ocular surface. IN: Pflugfeler SC, Stern ME, Beurman RW, editors. Dry eye and the ocular surface. New York: Marcel-Dekkar: 2004:11-40.

|
Kendra Davis, COA, is a senior ophthalmic technician for the Ocular Surface Center of Excellence at Bascom Palmer Eye Institute. Ms. Davis specialize in dry eye syndrome, meibomian gland dysfunction and Demodex folliculorum. E-mail her at dryeyeguru@gmail.com |








