Technology
Assessing penalties for MU, PQRS and VM
With penalties increasing, how much will it cost you to delay participation in these government programs?
BY KIMBERLY BALDWIN, MA, LPC
How much money will your practice lose if it does not implement a certified electronic health record technology (CEHRT) to achieve Meaningful Use (MU) and the Physician’s Quality Reporting System (PQRS) program? More than 440,000 eligible professionals (EPs) have received more than $20 billion in incentive funds for becoming meaningful users of CEHRT, according to CMS.gov. Unfortunately, your window for pursuing incentive funds is closed.
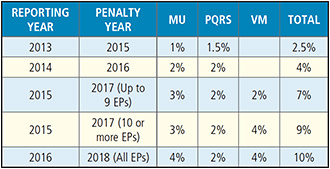
Also, you may see up to a 2.5% decrease in Medicare reimbursement this year based on your lack of reporting in 2013. By continuing to do nothing through 2016, you could be penalized a total of 10% of your Medicare payments in 2018. So, if your practice submits $100,000 in allowables for a provider, of which you would normally receive 80%, or $80,000, a 10% penalty would result in an $8,000 loss.
Figure 1 describes both the reporting year and the penalty year along with the penalties from Medicare for not participating in each of the programs. The percentage indicated applies to the allowable amounts submitted by the provider. For practices that continue to ignore these programs, the penalties will continue to rise this year.
Figure 1. Program penalties
MU penalties
The MU column in Figure 1 shows penalties for EPs choosing not to attest as meaningful users of CEHRT. If you decide to participate for the first time in 2015, you will need to attest to Stage 1 for a minimum of 90 days to avoid penalties for 2017. You will still receive the penalties this year for not attesting in 2013 and penalties in 2016 for failing to attest in 2014.
With CMS’ recent release of the final rule, you will need to review the 2015, Modified Stage 2 Rules. Also, see CMS’ guidance (http://tinyurl.com/OPpenalties1).
PQRS penalties
Along with incentive payments for participating in PQRS ending in 2014, choosing not to participate in the PQRS now results in 1.5% to 2% penalties. In 2015, PQRS is a full-year program and requires submission of nine measures from three of the six clinical quality domains and at least one cross-cutting measure. Participants may submit PQRS via claims or electronically through a registry such as the AAO’s Intelligent Research in Sight (IRIS), which qualifies for participation in both PQRS and the required Electronic Clinical Quality Measures (eCQMs) needed for MU.
Whereas the eCQM and MU programs focus on performing certain tasks, PQRS is strictly a reporting program. For example, you report that you performed a dilated eye exam on a diabetic patient. For more information, see CMS’ website (http://tinyurl.com/OPpenalties2).
Value modifiers
Even if you are making an informed decision to pay the MU and PQRS penalties, you must know that CMS’ penalties this year will go beyond programs that determine penalties based solely on whether you report. In 2015, “The Value-Based Payment Modifier (VM) Program evaluates the performance of solo practitioners and groups of practitioners, as identified by their taxpayer identification number, on the quality and cost of care they provide to their Fee-for-Service Medicare beneficiaries,” according to CMS.gov.
The Affordable Care Act mandated CMS to phase in this VM program, which provides for upward, downward or neutral payment adjustments to providers based on participation in the PQRS program. In 2015, the VM is applied to group practices of more than 100 EPs based on performance in 2013. In 2017, the penalties will apply to practices with soloists and groups of two to nine providers and groups with 10 or more EPs.
To determine the payment adjustments, CMS evaluates:
• Quality of the service provided. Reviewed by participation in PQRS.
• Cost of care provided. Evaluated by the CMS Physician Fee Schedule.
Payment is affected by not participating in PQRS or by the assigned quality tier made by CMS. For example, soloists and practices with two to nine EPs who opt not to participate in PQRS this year will automatically receive a 2% VM penalty — this is in addition to the 2% penalty they will receive for not participating in PQRS. Choosing to participate in PQRS for 2015, those same practices may receive no VM penalty or an upward adjustment of up to 2% based on the quality tier assigned by CMS. For more information, see the CMS’ website (http://tinyurl.com/OPpenalties3).
With the measures that relate to managing glaucoma, CMS will evaluate the quality of service you provide based on the measures you submit. For example, with measure 12, you document whether you performed an optic nerve head evaluation. For PQRS, it’s a matter of indicating whether you performed it or the medical reason for not performing. The VM program would rate you higher for performing the evaluation, contributing to your quality score.
Not all about penalties
When considering the cost of not participating in the various CMS programs, it’s also important to evaluate the cost of opting in. Take a good look at both the potential loss of revenue, in the form of penalties, and the investment required to purchase and implement a CEHRT. Consider the cost of purchasing the EHR, ensuring you have the appropriate IT infrastructure and hardware (servers, monitors, CPUs, tablets, scanners, printers, and more), training your physicians and staff, reducing your schedule to accommodate the learning curve of utilizing EHR, and the ongoing support fees of your vendor of choice.
Conclusion
You must decide if continuing to delay the transition to EHR is worthwhile. Now that you’re armed with more knowledge regarding the potential penalties, you can make an informed decision of whether you can continue to pay the penalties. OP

|
Kimberly Baldwin is a Licensed Professional Counselor in Colorado with a background in private practice ophthalmology, teaching, and community mental health. She currently works for the firm Destinations Consulting. |