Productivity
Are you getting the best ROI on staff? Measuring team performance
Learn how to crunch the numbers and quantify employee performance.
Maureen Waddle, Sacramento, Calif.
When you consider that approximately a quarter of every dollar coming into the practice goes back out to cover staff salaries, it is no wonder administrators and practice owners regularly evaluate their staffing models.
Determining the “right” amount to spend on staffing is a challenging, but necessary endeavor.
This article will review how managers can quantify and evaluate their investment in staffing.
Salary expense ratio
Managers can use several objective measures to make a case for either enhancing the staff or cutting back if the investment does not appear to be yielding desired results.
The salary expense ratio helps determine a reasonable staffing expense budget. Calculate the expense ratio by dividing the total gross salaries for all staff by the practice’s net collections (collections less refunds). Benchmarks gathered by BSM indicate most ophthalmology practices fall between 20–26% (that is the 25th percentile to the 75th percentile).
Predicting staffing needs
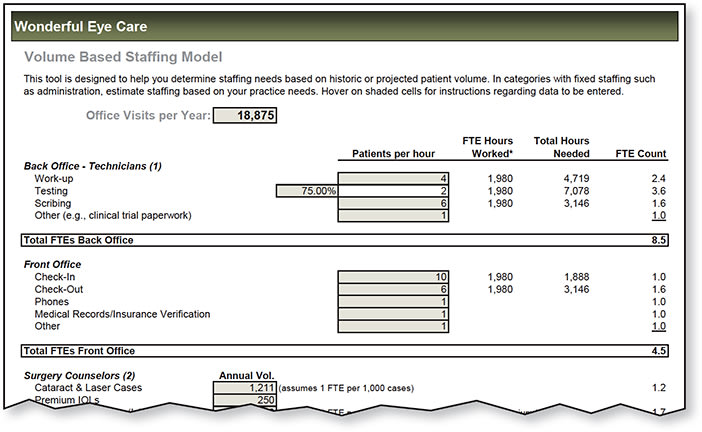
The number of full-time equivalent employees per full-time physician is a commonly used benchmark. The typical benchmark is five to eight full-time equivalent staff members per one full-time equivalent physician. However, this benchmark does have its shortcomings. For instance, it does not account for different subspecialties or practice patterns. Some ophthalmologists are comfortable seeing 70 patients per day while others prefer to keep the schedule around 40 patients per day. The volume of patients will certainly drive staffing demands. A volume-based model to predict staffing needs may be a better tool to help determine staffing requirements (Figure 1).
Figure 1: This Volume-based staffing model can help you predict staffing needs. For a look at the complete form, click here.
Beyond wages
Once you determine staffing needs and a baseline budget, you can then evaluate other staffing investments. Continuing education, for example, is a critical investment to enhance staff efficiency and create a productive work environment. To determine if your investment in continuing education for staff is worthwhile, monitor a variety of productivity measures for both individual staff members and the overall practice.
Enhancing productivity
Managers can measure the return on investments into staffing by establishing baseline productivity measures and other key staffing metrics. The idea is that investments, such as staff training, should improve productivity.
Or, perhaps you are trying to reduce staff turnover and decide to enhance a staff benefits package for a more competitive offering. Such a move that reduces staff turnover rates should also enhance productivity measures.
To establish these baseline productivity measures, consider the culture of your practice. For example, the net collections per full-time equivalent staff member may be high because the practice is understaffed. This will shrink the denominator.
Productivity measures
Other staffing measures will help you understand the complete picture. Productivity measures might include the following:
■ Patient visits per day per physician.
■ Patient work-ups per technician hour.
■ Reduction in errors. For technicians, this means fewer repeated diagnostic tests; for billing or front office staff, it means a reduction in claims error rates from data entry.
■ Net collections per full-time equivalent employee. This single measure is probably one of the most important to consider. Adding staff or training staff should be done to improve the efficiency of the physicians. It should improve collections. Calculate this number by dividing the practice’s net collections by the number of full-time equivalent staff. The range for this benchmark is $140,000–$190,000.
Staffing measures
If one of the practice goals for investing in staff is to create satisfied staff, consider measuring the items below. Decreases in absenteeism and turnover rates indicate your staffing programs are working well.
■ Absenteeism (sick leave/unplanned leave hours divided by total hours).
■ Turnover rate (number of staff members who left the practice during the year divided by number of positions).
■ Improved marks on staff satisfaction surveys.
■ Better patient interactions as recognized in regularly issued patient satisfaction surveys.
Owner’s opinion
A business manager is responsible for providing objective data to help owners make sound decisions. However, staffing greatly impacts the doctors, so the subjective side must be considered.
One last measure is to simply ask doctors about various staff members and if the training investment is improving the workday. The ultimate return in creating a satisfactory staffing model is a more pleasant and a measurably more productive practice. OP

|
Maureen Waddle |