Practice Management
Get Started With ICD-10
The new coding rules mean major changes. Here’s what you absolutely need to know.
Paul Larson, MBA, MMSc, COMT, COE, CPC, CPMA Atlanta
In less than a year, nearly all claims will require major changes. Starting on October 1, 2014, Payers are going to accept only ICD-10 diagnosis codes. (Only Workers’ Compensation claims are likely to remain in the familiar ICD-9 format, although even that may be temporary.) Imagine if all payments to the practice suddenly stopped. The result would obviously be devastating. Nothing quite so massive has happened to most of us in the field, since ICD-9 is the only code set we’ve known for diagnoses, but because the impact is that drastic, it’s important to have a strong background in ICD-10.
This article reviews what the new regulations will entail to help you begin preparing for the change.
ICD-10 Around the World
The payment system in the United States involves both Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. CPT is used mainly for office codes, tests, and surgeries when in the delivery of office-based services. Here, we also use it for proper claims filing and payment. Outside of the United States, ICD, with a few exceptions, is used to track public health, death and disease causes.
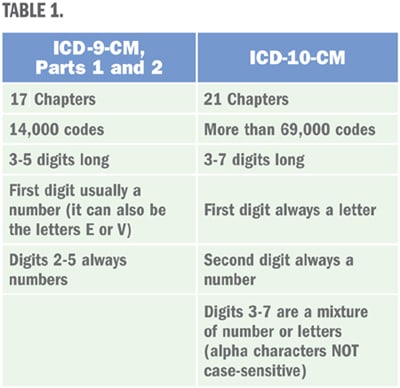
Almost the entire world converted to ICD-10 long ago. It was first proposed way back in 1993 and some countries went live shortly thereafter. ICD-10, like ICD-9, is divided into different parts. ICD-10 is divided into two parts; the “Clinical Modification,” or ICD-10-CM, and the hospital’s ICD-10-PCS “Procedural Coding System.” Both parts have the same implementation date. In the office setting (that means nearly all of us) we’ll be using ICD-10-CM. See Table 1 for some basic differences between ICD-10-CM and ICD-9-CM.
Differences Between ICD-9 and ICD-10
You’ll notice an incredible expansion in the amounts of codes. However, keep in mind that not every code is relevant to ophthalmology. The major difference you’ll see right away is the detail, or specificity, of ICD-10. For example: In ICD-9-CM, a patient with a central corneal ulcer, is coded 370.03. In ICD-10, however, that becomes:
▪ Central corneal ulcer, right eye (H16.011)
▪ Central corneal ulcer, left eye (H16.012)
▪ Central corneal ulcer, bilateral (H16.013)
▪ Central corneal ulcer, unspecif. eye (H16.019)
For eyelids, the differences are even starker. There are codes for each lid and eye as well as another one for unspecified lid/unspecified eye, a total of seven options!
Coding for Stage
Glaucoma will also see major changes. Coders will need to know the “stage” of the glaucoma for most codes. In ICD-9, you use 365.7x (“x” for the stage) in addition to the glaucoma type. In the case of a low-tension glaucoma patient (both eyes), coding staff must select 365.12 and then, based on the condition of the glaucoma, select the worst eye’s state to code. Under ICD-9, many offices do not bother noting the stages on claims. However, under ICD-10, no code will be possible without knowing the stage for each eye. In other words, there’s no option in ICD-10 to not know the stage. Additionally, attempting to use an unspecified code is not likely to work when ICD-10 rolls out. If OD is moderate and OS severe, you would need the two codes below to properly code the disease.
▪ Low-tension Glaucoma, right eye, moderate stage (H40.1212)
▪ Low-tension Glaucoma, left eye, severe stage (H40.1223)
How to Plan
First, review your charts. Do they have enough detail in the history, exam, and impression or plan to be able to choose a code in ICD-10? If not, that’s a great place to start — train individuals inputting chart information. They need to know a much higher level of specifics are needed. Use the previously mentioned examples to demonstrate.
Second, make a list of all the people (and software) who touch claims. You’ll find the list surprisingly long. It will likely include nearly everyone in the office. This demonstrates a valuable point to keep in mind: Many of the processes in your office will be severely affected unless everyone begins learning the new code set. Claims filing, PQRS, anything involving a prior authorization, your practice management system and your EHR systems are all impacted in major ways. Payers have been planning for ICD-10 for years and are way ahead of practices. There is time to catch up, however, as long as you don’t delay. OP
| Putting It off: Will ICD-10 be Delayed? |
|---|
|
In a word: No. Originally, this was slated to take effect October 1 2013. So, it was already delayed a year and the notice was given well in advance. When asked recently if there will be more delays, both current (CMS) Administrator Marilyn Tavenner and HHS Secretary Kathleen Sibelius have publicly stated there will be no further delays. In fact, in response to a December 2012 formal letter from the American Medical Association and more than 80 specialty physician associations (the AAO included) asking for a delay, CMS officially noted: “we believe that the one-year extension through September 30, 2014, offers physicians adequate time to train their coders, complete system changeovers, and conduct testing.” They also noted implementation would proceed as planned. |

|
Mr. Larson, MBA, MMSc, COMT, COE, CPC, CPMA, is a senior consultant at Corcoran Consulting Group. He specializes in coding and reimbursement. Mr. Larson is based in Atlanta.” |








