Dashboard
Use Performance Dashboard Reports to Help Maximize Operational Efficiency
This system helps your team focus only on those areas that directly drive practice results.
By Andrew Maller
In today's ophthalmology practice, operational efficiency is more important than ever. To be financially successful and well-positioned for the future, it is crucial that every person in a practice be as efficient as possible. This article introduces simple, easy-to-track performance metrics that each department—from the physician-owners to the front desk staff— can use to identify their operational weaknesses and strengths as they strive toward optimizing efficiency.
To measure efficiency, we develop a “dashboard.” Using an automobile analogy, a dashboard is an interface that organizes and displays key performance indicators (KPIs) to effectively gauge the health of a practice (or vehicle). Similar to car owners, practices should measure only that which is most important to overall health and performance. As a consultant, I typically recommend that each department track no more than three to five items, track them regularly, and use the results to identify opportunities for improvement. Following are several simple metrics that practices can track by department to ensure that their dashboards are fully functional.
DEPARTMENT: Front Desk/Reception
The front desk/reception staff is arguably one of the most important departments in the practice. It is responsible for handling all communication with new and established patients, making sure all sign-in and pre-authorization processes have been completed, and plays a major role in flow and efficiency in the office. That being said, the front desk dashboard report should track KPIs that measure patient flow and satisfaction. Here are a few examples (which are illustrated in the table “Front Desk/Reception Dashboard” below):
■ Patient No-Show Rate is calculated by dividing the number of no-shows for a period of time by the number of patients scheduled in that time period. When a patient fails to show up for a scheduled appointment for any reason, the practice is unable to generate revenue for that time. It is critical that the front desk develop protocols to minimize no-show problems. Consider tracking by new and established patients to identify patterns.
■ The Number of Patients Checked-In-per-Hour is measured by taking the total number of patients seen during a time period and dividing by the total number of hours worked by check-in personnel. Less-than-average results could indicate training opportunities for staff or inefficient new-patient registration procedures.
■ Average Patient Wait Time can be tracked by measuring the amount of time it takes once a patient checks in to when they are brought back for the examination. Track for a specified amount of time (e.g., one month) and then calculate an average for that period. Longer-than-average wait times could be the result of inefficient sign-in protocols, scheduling issues, or not being properly staffed during peak periods.
■ Tracking Patient Satisfaction is a must for all ophthalmology practices. Results can be used to assess patient satisfaction levels of the initial phone conversation and the check-in and check-out processes. After measuring patient satisfaction for a specific amount of time, practices will be able to establish benchmarks in these areas and set goals to either maintain or exceed the benchmark. Regularly review scores to identify training opportunities related to telephone and general customer service skills.

|
||||
| Front Desk/Reception Dashboard - Sample Practice 1 | ||||
| RESULTS | June2011 | June 2012 |
Variance | Goal |
| Patients Scheduled | 815 | 775 | -40 | |
| Patients Seen | 780 | 725 | -55 | |
| No-Shows | 30 | 42 | 12 | |
| Front Desk Hours Worked | 260 | 205 | -55 | |
| EFFICIENCY RATIOS | ||||
| Patient No-Show Rate | 3.7% | 5.4% | 1.7% | Less than 3% |
| PatientsChecked-In-per-Hour | 3.0 | 3.5 | 0.5 | 5 |
| Average Patient Wait Time (Minutes) | 15 | 20 | 5 | Less than 15 |
| Patient Satisfaction Score (1-5 Scale) | 4.30 | 4.05 | -0.25 | 4.5 or Greater |
DEPARTMENT: Clinical
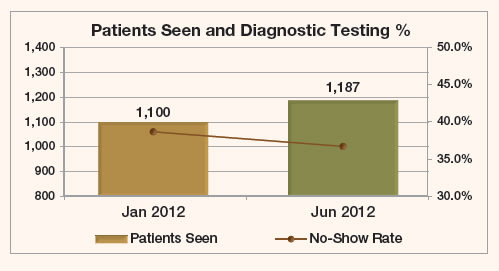
The clinical staff plays a critical role in managing patient flow and satisfaction in the exam lanes. More than any other position in the practice, technicians can have the greatest impact on keeping the doctors on schedule and limiting patient wait times. The following list, illustrated in the table “Sample Practice 2 – Clinic Department Dashboard,” (right) includes a sampling of the many metrics that clinic staff can track to ensure that patients are efficiently seen without sacrificing patient care and overall satisfaction.
■ Exam Work-Up Time should periodically be measured to ensure that patients are being prepped for the doctor in an efficient manner. National benchmarks indicate that, on average, it takes a technician approximately 15 minutes to perform an exam work-up that includes a refraction. While the amount of time will vary based on specialty and practice model, it is important to track the results to compare against practice results over time.
■ Total Exam Time should also be tracked often in order to assess overall doctor-staff flow and efficiency. Start the clock when the patient is called in from the waiting area, and stop it when they get to the checkout area. Try to segment each part of the process, including the time it takes to walk to the exam room, the work-up time (see Exam Work-up Time), and the actual exam with the doctor. Higher-than-average times can indicate patient-flow issues, exam lanes not being properly equipped, and/or technician or scribe training opportunities. Remember that every second counts and the most successful practices look to create processes that maximize the efficiency of the doctor.
■ Total Number of Patients Seen Per Hour is important to track as it provides a barometer of determining clinical staffing needs. To track, take the total number of patients seen during a period of time, and divide by the total number of hours worked by clinical staff. For practices with multiple providers, consider tracking by individual doctor to determine appropriate staffing levels.
■ The Diagnostic Testing Percentage measures the number of tests ordered divided by total office visits. Some (but not all) diagnostic tests include visual field examinations, OCTs, A-Scans, and HRTs. While this will vary by subspecialty, measuring the number of tests compared to office visits provides a useful way to gauge technician training opportunities and staff scheduling.
|
||||
| Sample Practice 2- Clinic Department Dashboard | ||||
| RESULTS | Jan 2012 | Jun 2012 | Variance | Goal |
| Total Patients Seen | 1,100 | 1,187 | 87 | |
| Diagnostic Tests Performed | 425 | 435 | 10 | |
| Technician Hours Worked | 550 | 570 | 20 | |
| EFFICIENCY RATIOS | ||||
| Average Exam Workup Time (Minutes) | 17 | 21 | 4 | 15 Min or Less |
| Average Exam Time (Minutes) | 28 | 32 | 4 | 30 Min or Less |
| Patients Seen per Hour (By Technician) | 2.0 | 2.1 | 0 | 3 or More |
| Diagnostic Testing Percentage | 38.6% | 36.6% | -2.0% | |
DEPARTMENT: Billing and Collections
The billing and collections department controls the flow of money into the practice. It is responsible for posting charges and payments, accurately completing claims, and working with third-party payers and patients to ensure that money owed to the practice is collected in a timely manner. With this in mind, I recommend tracking the following KPIs to make sure this department is operating as efficiently as possible. (See the table “Billing and Collections Dashboard - Sample Practice 3” below.) The information required to track these metrics should be easily available in all practice management systems.
■ The Claims Error Rate is calculated by taking the total number of claims errors (claims kicked out during the electronic claims prep process plus claims denied due to errors in data entry) and dividing by the total claims submitted during the given time period. If more than 20% of claims submitted are denied, it is important to identify patterns in an effort to locate the source of the errors. They are often traced to incorrect coding and entering inaccurate patient demographic and insurance information. Once identified, conduct staff training related to problem areas.
■ Net Collection Ratio is calculated by taking the professional fee net collections during a specific period of time and dividing by adjusted charges (gross charges less adjustments and write-offs). This ratio represents the practice's ability to collect that which it is legally entitled to. The benchmark for this ratio is 95—99%.
■ Days Sales Outstanding (DSO) (see calculation below) is a measure of how quickly receivables turn over in the practice. DSO is calculated by dividing the adjusted accounts receivable by average daily collections (illustrated in the following formula). The result for healthy practices, expressed in days, is typically between 25—45 days. A high number of days may indicate billing, collection, or potential payer issues. Keep in mind that practices with a high percentage of revenues that are paid up front (due to cosmetic surgery, premium IOL fees, or refractive surgery) often have a lower DSO.
| DSO | Adjusted Accounts Receivable Balance(Current A/R balance × gross collection ration (net collections/gross charges)) |
| Average Daily Collections(Net collections/number of days in the time period) |
■ Accounts Receivable Aging Analysis (see table below) is a report that most (if not all) practice management systems already track. It is measured by taking the A/R balance for a specific day range and dividing by total accounts receivable. Aberrant percentages in the following day ranges can be caused by billing problems or payer delays.
| Accounts Receivable Aging Category | Percent of Accounts Receivable Total |
| 0—30 Days | 40—60% |
| 31—60 Days | 15—25% |
| 61—90 Days | 5—10% |
| 91—120 Days | 5—10% |
| Over 120 Days | 10—20% |

|
|||
| Billing and Collections Dashboard - Sample Practice 3 | |||
| RESULTS | Jun 2011 YTD | Jun 2012 YTD | Variance |
| Total Charges | $10,636,976 | $10,689,635 | $52,659 |
| Total Adjustments | $6,098,639 | $6,136,436 | $37,797 |
| Net Collections | $4,363,639 | $4,298,636 | -$65,003 |
| Claims Submitted | 31,636 | 31,986 | 350 |
| Claim Errors | 3,656 | 4,263 | 607 |
| FINANCIAL METRICS | |||
| Claims Error Rate | 11.6% | 13.3% | 1.8% |
| Net Collection Ratio | 96.2% | 94.4% | -1.7% |
| Days Sales Outstanding | 26 | 32 | 5 |
| ACCOUNTS RECEIVABLE AGING ANALYSIS | 6/30/2011 | 6/30/2012 | Healthy Range |
| 0 - 30 Days | $1,063,693 | $1,163,696 | 40% - 60% |
| 31 - 60 Days | 215,636 | 415,636 | 15% - 25% |
| 61 - 90 Days | 75,636 | 65,636 | 5% - 10% |
| 91 - 120 Days | 54,636 | 43,636 | 5% - 10% |
| Over 120 Days | 115,636 | 165,363 | 10% - 20% |
| Total Accounts Receivable | $1,525,237 | $1,853,967 | |
How to Use Results
After baselines have been created, owner-physicians and practice managers should join forces with specific departments to establish measurable goals to improve performance. In addition to being linked with the overall objectives for the practice, goals should be time-specific and attainable. Some examples are:
■ The front desk will achieve a 30% reduction in the patient no-show rate within 90 days.
■ The average exam work-up time will remain at or below 15 minutes.
■ The billing and collections department will increase the net collection ratio to 95% or greater by the end of the year.
Once goals have been established, continue to track the results on the department dashboard and identify opportunities for improvement.
Look to Improve
The metrics described in this article are valuable tools that reflect just a few of the many areas that can be tracked to identify operational strengths and weaknesses. For optimal success, though, a practice must focus most on areas that directly drive practice results. Start simple by tracking a few items to avoid becoming overwhelmed and losing focus of the big picture. Practices that continually look to improve processes and protocols will be ready to conquer the challenges of the future. OP

|
Andrew Maller, Associate Consultant BSM Consulting works out BSM Consulting's Scottsdale, Arizona office. He assists with development of practice management tools and resources and financial benchmarking programs. He also assists with client projects across BSM's areas of health specialties. |








